The term osteochondrosis itself is derived from two words: osteo - bone and chondrue - cartilage. Simply put, it is the ossification of the cartilage. Although this interpretation is fundamentally wrong. Some in their delusions go even further and trust that osteochondrosis is the deposit of salts in the joints. Furthermore, it is table salt that is supposedly consumed in large quantities as food.
Pathogenesis
In reality, everything happens a little differently. And harder. And table salt, if it plays any role in the appearance of osteochondrosis, is very indirect. Osteochondrosis is based on the degeneration and degeneration of articular cartilage. This is not an independent disease, but a pathological process that can be observed almost anywhere where there is connective cartilage tissue.
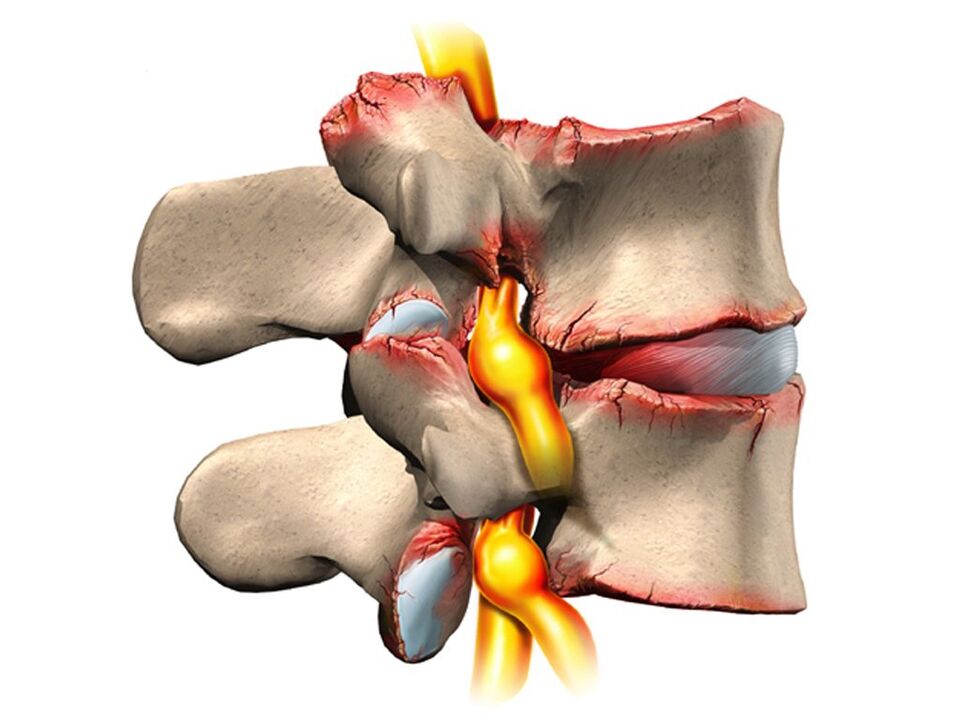
Still, osteochondrosis in the overwhelming case affects the spine. Why is that? The fact is that between the vertebrae there is a kind of pads - intervertebral (intervertebral) discs. The physiological function of these discs is to cushion and protect the vertebral bodies from premature wear due to mechanical stress. The disc consists of an internal liquid nucleus pulposus surrounded by an annulus fibrosus and an upper and lower end plate.
The disc undergoes tremendous mechanical stress, causing permanent damage to its structures at the cellular level. In humans, these processes are too pronounced - this is our pay for walking upright. To prevent the disk from being "erased" completely, it must constantly regenerate itself, that is, rebuild itself. It is the balance of the regenerative processes of damage that determines the normal structure of the intervertebral disc. Another curious detail is that the supply of blood and nutrients to the intervertebral discs is not carried out through the blood vessels, which grow too large in childhood, but diffusely, from the bone tissue of the vertebral bodies. Again, paying for the ability to move on two limbs, not four.
Due to this, the intervertebral discs are easily injured in anatomical and physiological terms. Any negative process in the body leads to an imbalance in the damage-regeneration balance and the development of dystrophy and degeneration in the discs. A structurally defective disc can no longer withstand adequate mechanical stress. Under excessive pressure from the overlying vertebrae, the discs shift in different directions, usually to the sides and back. This process is called a herniated disc.
The bone tissue of the vertebrae, which has lost its cartilage lining, also undergoes mechanical wear. Due to constant trauma to the surface of the anterior border of the vertebral bodies, pathological bone growths are formed - osteophytes. Spondylosis develops. Due to the degeneration and displacement of the disc, the intervertebral spaces diminish, the spinal canal narrows and the roots of the spinal nerves are infringed in the so-called foraminal foramen.
Causes
The causes or etiological factors of osteochondrosis are diverse. They can be both local, that is, due to the pathology of the spine itself, and general disorders at the level of the organism. Any pathology that leads to a violation of the structure of the spine or metabolic disorders can be considered as the cause of osteochondrosis. In this regard, there are:
- Changes in the configuration of the spine (scoliosis, pathological lordosis or kyphosis).
- Other defects of the musculoskeletal system are flat feet, narrow shoulder girdle, abnormalities in the structure of the pelvis.
- Spinal injury.
- Weak immunity.
- Metabolic disorders: osteoporosis, obesity, diabetes mellitus, thyroid disease.
- Diseases of the cardiovascular system: atherosclerosis, hypertension.
- Digestive disorders leading to insufficient absorption of nutrients from the gastrointestinal tract.
- Inheritance.
It should be noted that the above pathological conditions do not necessarily lead to osteochondrosis. This requires constant exposure to certain predisposing factors: hypothermia, malnutrition, a sedentary lifestyle or, conversely, excessive physical effort.
Symptoms
Osteochondrosis itself is an asymptomatic process. And at the same time, the signs of degeneration of the intervertebral disc are diverse. How is that? The fact is that the clinical manifestations of osteochondrosis are based on its complications: herniated discs, spondylosis, sciatica, narrowing of the spinal canal.
In addition, the symptoms are highly variable depending on the predominant location of the process in the cervical, thoracic or lumbosacral spine. The last section is the most affected, since it is the lower back that performs the maximum physical activity. Signs of osteochondrosis of the lumbosacral region:
- Pain (lumbodynia, lumbago, sciatica).
- Restriction of movement in the lower back and lower extremities (intermittent claudication).
- Here, the sensitivity disorders of the type of paresthesia: numbness, burning, tingling.
- Pathological tension of the lumbar muscles.
- In the absence of treatment, disorders of the function of the pelvic organs.
Cervical osteochondrosis is seen less frequently than lumbosacral. However, this pathology is also quite common. In addition to the typical signs of pain (neck pain), decreased sensation and movements in the upper extremities, cervical osteochondrosis due to poor blood supply to the brain has its own characteristics. These characteristics are manifested:
- Insomnia.
- Headache, dizziness.
- Periodic nausea
- General weakness, rapid fatigue.
- Blood pressure fluctuations.
- Occasionally toothache.
- Behavioral reactions in the form of crying, irritability.
The thoracic region with osteochondrosis is affected relatively infrequently. Patients in this case are people forced to sit in a fixed awkward position by occupation: students, schoolchildren, programmers, office workers. The symptoms of osteochondrosis in this case will be as follows:
- Pain and paresthesia in the chest.
- Dyspnoea
- Heartbeat sensation.
- Restriction of movement in the thoracic spine.
Diagnostics
From all this it is clear that osteochondrosis is a chameleon disease. Due to the similarity of signs, it is easy to confuse it with stroke, hypertension, myocardial infarction, angina pectoris, neurotic disorders. That is why, in order to make the correct diagnosis, a comprehensive complex diagnosis is necessary to correctly determine the symptoms and treatment of osteochondrosis.
This diagnosis, in addition to the traditional questioning and clarification of patient complaints, must include a medical examination and special investigation methods. These methods include X-rays of the spine, ultrasound of internal organs. Recently, computerized and magnetic resonance imaging have been used with success to diagnose osteochondrosis.
Treatment
Therapeutic tactics for osteochondrosis involve the use of:
- Medicines.
- Massage.
- Physiotherapy procedures.
- Physiotherapy (exercise therapy).
- Manual therapy.
- Acupuncture.
Medication for osteochondrosis is primarily aimed at relieving pain and eliminating inflammatory processes in the nerve roots. In various combinations, these drugs are widely used in the form of ointments, injections, tablets for the treatment of osteochondrosis. It should not be forgotten that these drugs have a negative effect on the liver, stomach and intestines. By this, they can aggravate metabolic disorders in osteochondrosis. They relieve the pain of the block well with local anesthetics. True, the effect of these funds is short-lived and in no way affects the course of osteochondrosis as a whole.
It is possible to improve metabolic processes locally and in the body with the help of drugs such as chondroprotectors, immunostimulants and vitamins with minerals. Chondroprotectants are used in tablets, ointments, and ampoules. Among the fortifying agents, vitamins C, group B, are used in combination with minerals. In this regard, calcium preparations are most preferred. In fact, contrary to some erroneous claims, the basis of osteochondrosis is not an excess, but only a deficiency of calcium.
After successfully relieving the exacerbation, physiotherapy, massage and exercise therapy procedures are shown. As physical procedures, calcium electrophoresis, hydrocortisone phonophoresis, amplipulse, paraffin therapy are used. All these measures are aimed at eliminating pain and inflammation in the nerve roots, ligaments and muscles. Massage for osteochondrosis is carried out according to the generally accepted method. The massage zone is selected depending on the location of the osteochondrosis. Expansion of range of motion is achieved with the help of exercise therapy. At first, in the exacerbation phase, there are practically no dynamic loads. The patient is constantly in an optimal posture. At this time, it is desirable to use immobilization devices - a lumbar corset, Shants neck. As the exacerbation subsides, the volume and duration of movements increases during exercise therapy.
Recently, in the treatment of osteochondrosis, non-traditional treatment methods have been received: acupuncture, manual therapy, osteopathy. Acupuncture is an effect on special biologically active points located along the spine, in the atria, on the hands and on the feet. With manual therapy, the normal position of the vertebrae and intervertebral discs is restored through the manual action of the hands of a specialist. And in the course of osteopathy, the structural integrity of the musculoskeletal system is ensured by specific techniques. In the absence of the effect of conservative measures for the treatment of osteochondrosis, persistent pain, complications, surgery is indicated. The pathologically displaced disc is removed. Currently, for this purpose, a microdiscectomy is performed - endoscopic removal of a displaced disc.















































